Feline hyperthyroidism was first described as a spontaneous disease in 1979. Shortly thereafter it became recognized as the most common endocrine disorder of the cat. The elevated circulating levels of the thyroid hormones thyroxine (T
4) and triiodothyronine (T
3) that occur in hyperthyroidism result in a multisystemic disease.
The most commonly recognized signs of hyperthyroidism are weight loss, hyperactivity, and an increased appetite. An increased water consumption and urination are other common signs of feline hyperthyroidism that are thought to result from an increased blood flow to the kidneys. Gastrointestinal signs are common in hyperthyroidism. Intermittent vomiting and diarrhea are frequently noted. Cardiovascular signs including an increased heart rate, arrhythmias and congestive heart failure, are common in cats with hyperthyroidism. Most cats with hyperthyroidism develop a reversible form of heart disease with congestive heart failure developing in 10 to 15% of these cats. Apathetic hyperthyroidism represents an unusual form of hyperthyroidism that occurs in approximately 10% of cats with hyperthyroidism. In these cats, the typical signs of hyperactivity and increased appetite are replaced by depression and inappetance. Weight loss may progress at an enhanced rate in these cats. In addition to these nonspecific signs, a majority of hyperthyroid cats will have an enlarged thyroid gland.
Clinical Signs
Feline hyperthyroidism occurs in middle-aged to old cats with no breed or sex predilection. The clinical signs of hyperthyroidism may vary from extremely mild (in some cases no clinical signs are recognizable) to severe. The multisystemic effects of hyperthyroidism result in signs that reflect dysfunction in many organ systems. The clinical signs usually reflect the stimulatory nature of thyroid hormones on the various organ systems.
Diagnosis
The diagnosis of feline hyperthyroidism is routinely made based on the measurement of elevated circulating levels of the thyroid hormones thyroxine (T
4) and triiodothyronine (T
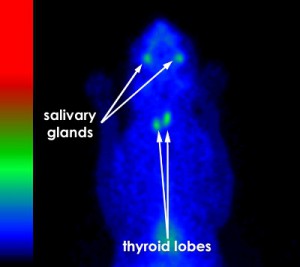
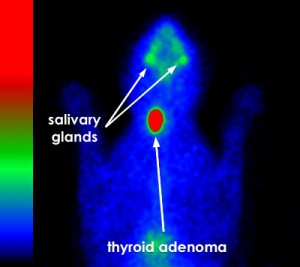
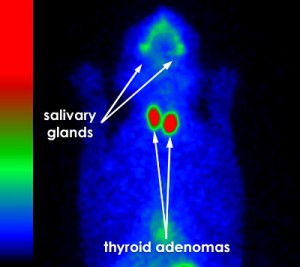
3). However thyroid hormone concentrations in cats with hyperthyroidism are subject to significant variation over time. Planar thyroid scintigraphy (or thyroid imaging) is useful in the detection of the hyperfunctional thyroid tissue that causes the disease. The major value of thyroid scintigraphy is determining the extent of the thyroid gland involvement. Thyroid scintigraphy is also invaluable in the evaluation of the thyroid carcinoma patient.
Therapy
The therapy for hyperthyroidism is directed at controlling the excessive production of thyroid hormones. Four options for therapy are available; 1.) antithyroid drug administration, 2.) iodine deficient diets, 3.) surgery, and 4.) radioactive iodine. Of these therapies, the most recent is the newly developed Iodine deficient diet that has been shown to lower circulating thyroid hormone levels in hyperthyroid cats. When used to treat hyperthyroidism, strict adherence to these diets is required, as even small amounts of regular cat food will negate their effect. Because these diets require lifetime administration and should not be fed to cats with normal thyroid function, multi-cat households may experience difficulty with this form of therapy. Antithyroid drug administration will inhibit the synthesis of thyroid hormones.Methimazole (Tapazole
®) is currently the antithyroid drug of choice. Antithyroid drug therapy is lifetime with symptoms of the disease recurring rapidly following discontinuation of the drug. Surgical thyroidectomy is a highly effective therapy for feline hyperthyroidism. Unfortunately anesthetic and surgical complications can result in significant morbidity and mortality. Greater than 70% of the cats with hyperthyroidism have bilateral thyroid involvement. In cats with bilateral thyroid involvement, removal of both lobes is necessary to control hyperthyroidism. Post-operative complications include hypoparathyroidism, Horner's syndrome, laryngeal paralysis and persistent hypothyroidism.Radioactive iodine
131I therapy is currently the therapy of choice in most cases of feline hyperthyroidism. Radioactive iodine is preferentially concentrated in the adenomatous areas of the thyroid while the normal thyroid tissue takes up relatively little iodine due to normal feed back suppression. The ß (beta) particle emitted by
131I travels an average distance of 400 µm. This treatment is therefore locally destructive but spares the adjacent hypoplastic (normal) thyroid tissue as well as the parathyroid and other cervical tissues. Radiation safety precautions require that cats remain hospitalized following their
131I therapy until they have eliminated a majority of the radioactive iodine from their bodies. This typically requires a hospitalization of 3 to 7 days. Radioactive iodine therapy is considered the optimum treatment for feline hyperthyroidism. It involves a single nonstressful procedure that is without associated morbidity or mortality. Significant side effects have not been observed. Unlike surgery, anesthesia is not necessary. A single dose of radioactive iodine will result in a return to persistent euthyroidism (normal thyroid function) in a majority (>95%) of cats with hyperthyroidism. Since the cats's thyroid function returns to normal following
131I therapy, no ongoing thyroid medications are needed following this form of treatment. The logistics surrounding radioiodine therapy for cats with hyperthyroidism have dramatically changed since it was first reported in the veterinary literature in 1984. A
brief historical editiorial of the changes that have developed over the last 20 years at AVMI including the addition of Snyder Cat Cottages and personal iCat web cams is available.