Etiology
Nonhemorrhagic infarctions, otherwise called ischemic infarctions, are the result of the acute interruption of blood flow to an area within the brain. The usual cause for a nonhemorrhagic infarction is the occlusion of an intracranial artery by a thromboembolism. Nonhemorrhagic infarctions differ from hemorrhagic infarctions that are associated with intraparenchymal brain hemorrhage.Pathophysiology
Acute reduction of blood flow to a region of the brain leads to ischemia. Cytotoxic edema ensues secondary to cell death. Subsequent disruption of the blood brain barrier leads to an influx of water and proteins into the intracellular space causing vasogenic edema within 4-6 hours of the event that can continue for 3-5 days thereafter.Clinical Signs
Clinical signs associated with nonhemorrhagic infarctions can include mentation changes, circling, and seizures for cerebral infarctions; hemi- or tetra paresis and cranial nerve deficits for brain stem infarctions; as well as vestibular signs for cerebellar infarctions. While the exact nature of the symptoms that occur vary with the location of the infarction, a key to the diagnosis is the acute nature of the onset of symptoms combined with the relative lack of progression shortly following their onset.Diagnostic Tests
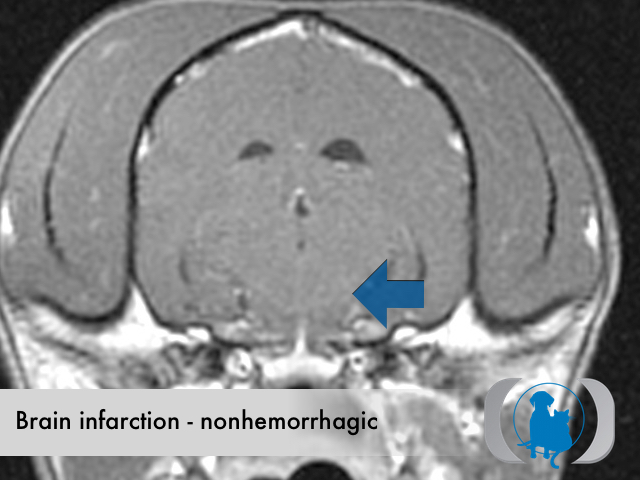
MRI is the diagnostic imaging modality of choice for diagnosing nonhemorrhagic infarctions. Nonhemorrhagic infarctions are hyperintense on FLAIR and T2 weighted images, hypointense on T1 weighted images, and demonstrate a poor, heterogeneous and frequently exclusively peripheral enhancement following contrast. The extent of contrast enhancement is related to the revascularization of the brain and hence driven by the time interval between onset of symptoms and imaging. Additional MRI sequences including perfusion, diffusion and magnetic resonance angiography can provide additional useful information in cases with nonhemorrhagic infarction.Therapy
Therapy for nonhemorrhagic infarctions includes largely symptomatic therapy for seizures and the potential concurrent ataxia and paresis that may occur pending the location of the infarction. When possible, therapy directed at the cause of the infarction should be pursued. Unfortunately in most cases of nonhemorrhagic infarction in dogs and cats, the underlying cause for the infarction is not identified.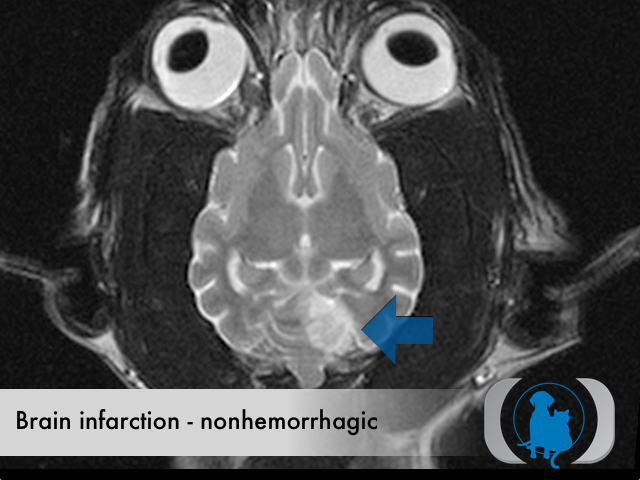
Dorsal plane T2 weighted MRI of the brain of a 12 year old Terrier mix dog showing a left sided, nonhemorrhagic cerebellar infarction (blue arrow).
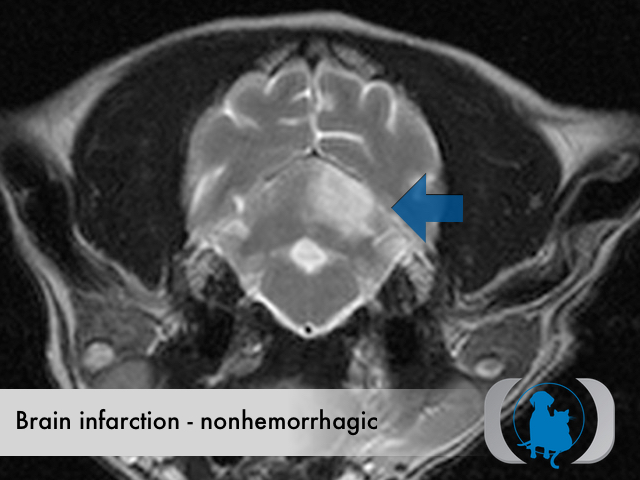
Axial plane T2 weighted MRI of the brain of a 12 year old Terrier mix dog showing a left sided, nonhemorrhagic cerebellar infarction (blue arrow).
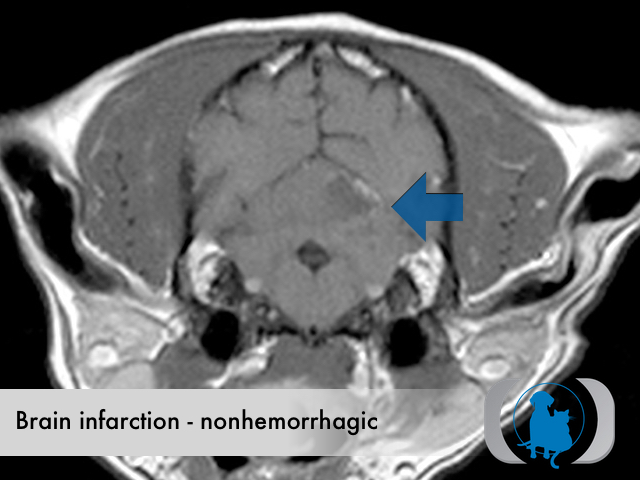
Dorsal plane post contrast T1 weighted MRI of the brain of a 12 year old Terrier mix dog showing a left sided, nonhemorrhagic cerebellar infarction (blue arrow).
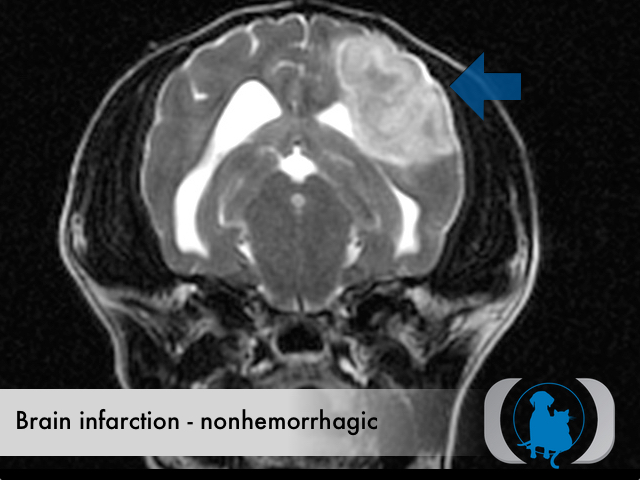
Axial T2 weighted MRI of the brain of a 13 year old Yorkshire Terrier dog with a nonhemorrhagic infarction of the left cerebrum (blue arrow).
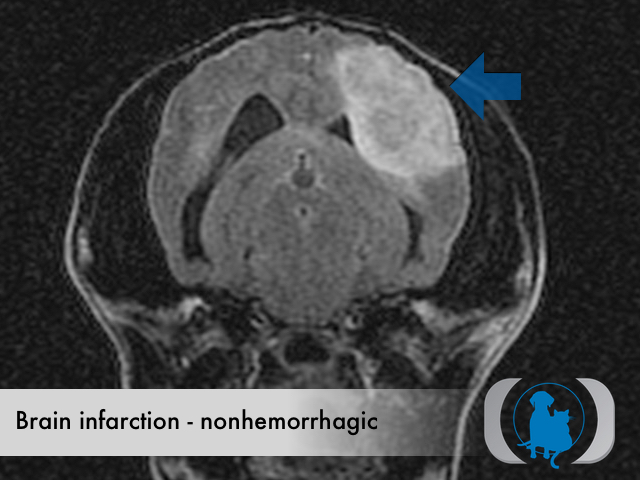
Axial FLAIR MRI of the brain of a 13 year old Yorkshire Terrier dog with a nonhemorrhagic infarction of the left cerebrum (blue arrow).
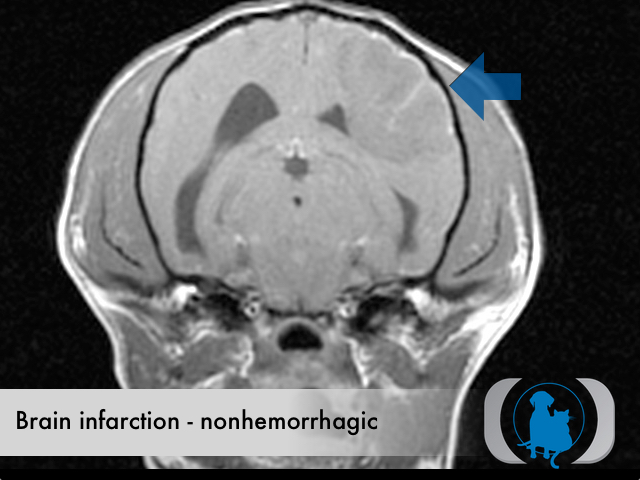
Axial post constrast T1 weighted MRI of the brain of a 13 year old Yorkshire Terrier dog with a nonhemorrhagic infarction of the left cerebrum (blue arrow).
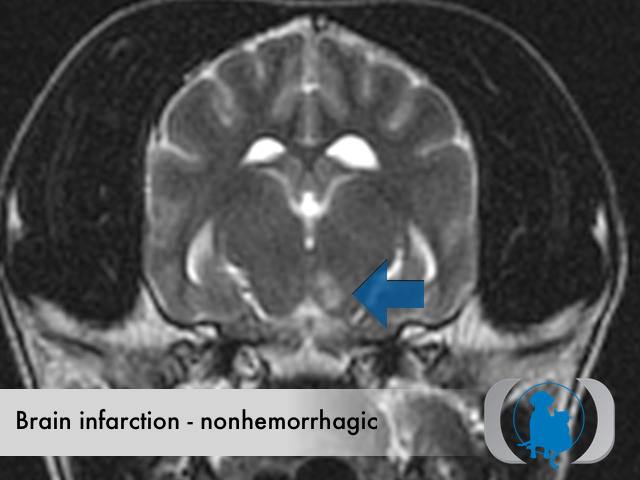
Axial T2 weighted MRI of the brain of a 10 year old Australian Shepherd dog with a nonhemorrhagic infarction of the left thalamus (blue arrow).
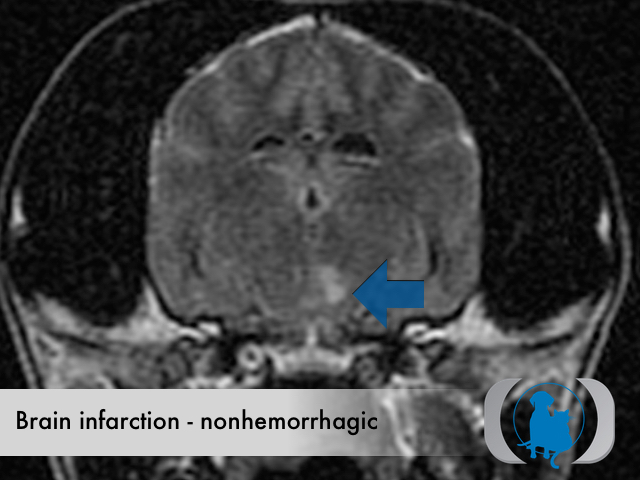
Axial FLAIR MRI of the brain of a 10 year old Australian Shepherd dog with a nonhemorrhagic infarction of the left thalamus (blue arrow).
Axial post constrast T1 weighted MRI of the brain of a 10 year old Australian Shepherd dog with a nonhemorrhagic infarction of the left thalamus (blue arrow).

