Etiology
Aspergillosis is the result of infection by one of several different species of the saprophytic fungi of the genus Aspergillus. While there are hundreds of different species of Aspergillus, the most common causes for infections of the dog and cat are Aspergillus flavus, Aspergillus fumigatus, Aspergillus nidulans and Aspergillus niger. While cases of Aspergillosis occur in the cat, the infection is much more common in the dog. These fungi are ubiquitous in the environment as frequent contaminants of food products and potentially representing major components of mildew. As a results Aspergillosis can occur anywhere in the world. Young dogs with a medium to long nose conformation (meso or dolichocephalic) are overrepresented.
Pathophysiology
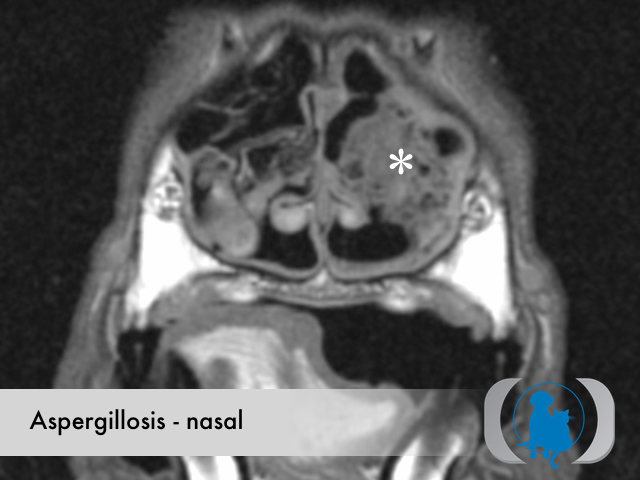
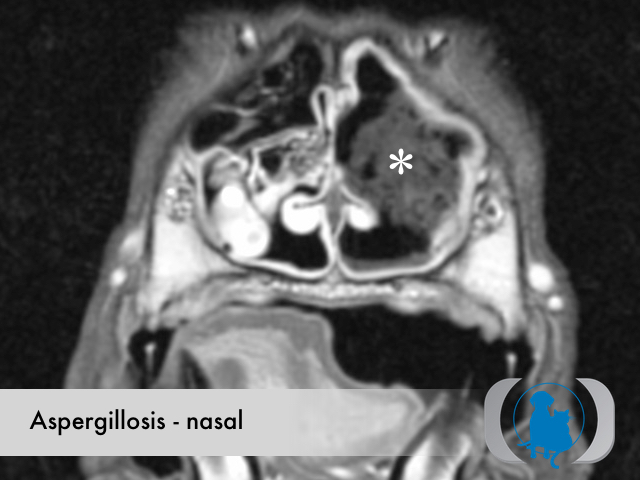
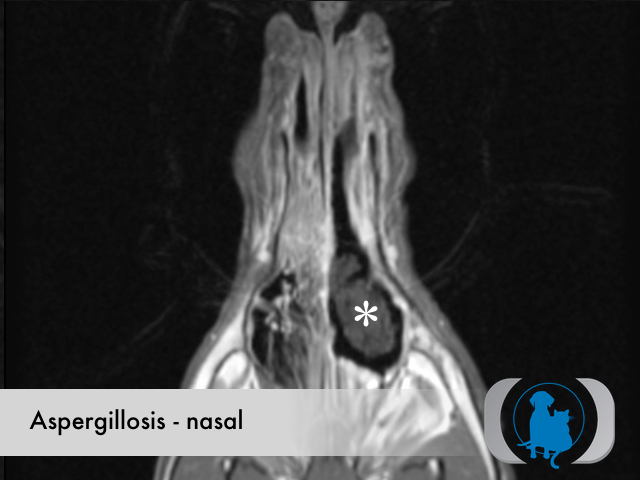
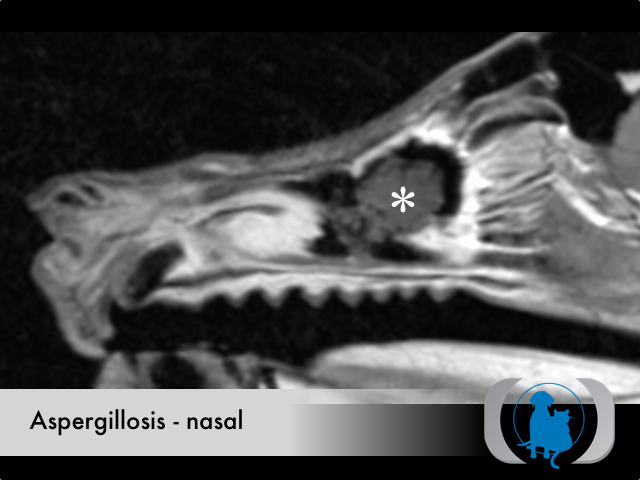
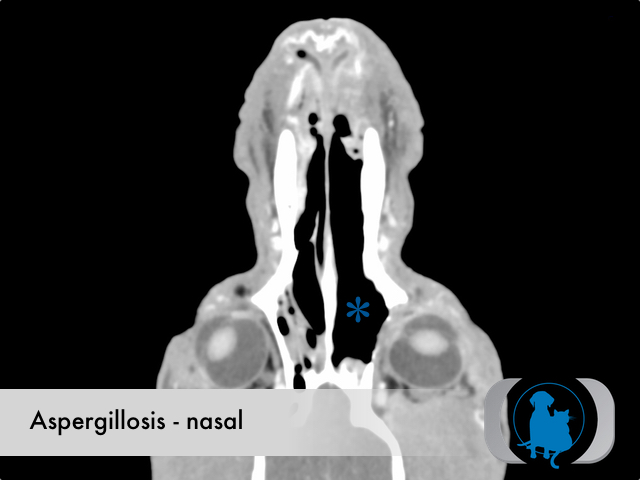
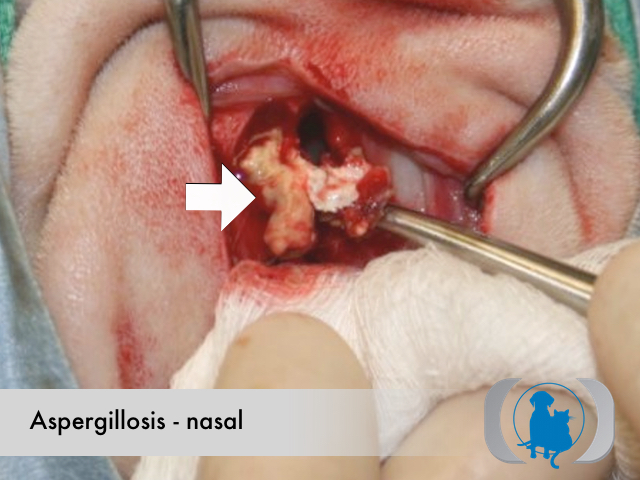
The infectious form of the fungus called conidia, are routinely inhaled and infrequently overcome the local immune response leading to colonization of the nasal cavity and/paranasal sinuses of the dog and much less frequently the cat. The colonization can lead to large aggregates of organisms within the lumen of the nasal cavities or sinuses called aspergillomas, otherwise known as mycetomas or fungal balls. The persistent presence of the fungus within the nasal cavity leads to chronic stimulation of the local immune system resulting in potentially dramatic lysis of the turbinates underlying the nasal mucosa. Facial bone lysis and/or osteitis, especially involving the bones around the frontal sinuses, are a common finding in patients with this disease.
Clinical Signs
With nasal Aspergillosis the clinical signs reflect the localization of the infection within the nasal cavity. Chronic immune stimulation leads to diffuse nasal mucosal thickening and congestion as well as chronic mucopurulent or hemorrhagic nasal discharges. Sneezing, pawing at the muzzle and a stertorous respiratory pattern are common manifestations. With more severe forms of the disease, extension into surrounding tissues can lead to periorbital swelling, distortion of the overlying facial conformation and rarely CNS symptoms.
Diagnostic Tests
Serologic testing for antifungal antibodies and cultures of nasal discharges or swabs are confounded by frequent false negative and false positive results. Identification of organisms within biopsy samples from infected nasal mucosa can be diagnostic. Even biopsy samples however may reveal only the marked lymphoplasmacytic inflammatory response elicited by the infection. Direct visualization of the diffuse mucosal thickening, extensive turbinate lysis and aspergillomas with rhinoscopy and/or advanced diagnostic imaging (CT and MRI) are frequently required to confirm the diagnosis.
Therapy
Systemic antifungal drugs play a role in treating cases with extension of the infection beyond the nasal cavity (i.e., subcutaneous facial tissues or orbits). Systemic therapy alone is rarely effective however and administration of 1 of several different topical antifungal therapies (i.e., clotrimazole, enilconazole, bifonazole) is generally required. These topical therapies require prolonged general anesthesias during which time the nasal mucosa is coated by submersion.
Image Gallery